Case refered by Dr. Mukesh Ladda from nagpur for opinion.
Please give your views and comments
54yr male diabetic presented with bilateral stiff hip since one yr,slowly progressive to total stiffness since last six months.
History of septicemia with multiorgan failure one n half yr ago,recovered well but unable to stand or sit due to bilateral stiff hip.
His question are as follows? My comments below are open to your valuable comments and views
1.Is THR only option?
With the sort of long standing Ankylosis the articular cartilage nutrition suffers and result in fibrous or bony ankyloisis. The question whether this was the result of septic arthritis or due to neuraxial injury could be partly answered by ESR, CRP and intraop frozen section. Being a diabetic an HBAIC is advised. IF proven to be infected could consider girdlestone with local antibiotic delivery could be a choice before THR. If not A THR with the largest possible head to avoid dislocation
2.What will be the status of Abductors after removing HO?
I would go dead lateral, split the TFL with anterior and posterior with bone slivers from the G. Troch. Do a neck ostetomy and remove the head, Ream or piece meal. After this the bone anterior and posterior can be removed slowly exposing the bone subperiosteally and reove all the impinging bone. You want to watch for N/V damage palpating vessels and preop MRI angio if needed to asses where the vessels are embedded if needed. The all important homan's retractor, electroquatery helps exposing the HO. The one similar case i did had a compartmental syndrome of thigh and femoral neurpraxia which recovered partially in 6 months. The contralateral hip was done 6 months later and laser was used toquarterise the bleeding bone to avoid compartmental syndrome. Those days we did not have any local thrombin delivery to stop bleeding if possible.
3.When should i do the second hip(gap between two THR)?
I would wait 3 to 6 months only for recovery
4.What are the chances of recurrence? In my only experience of a bilateral case the xrays below the hip failed with a psuedo tumor due to MOM articulation with an XL head.
5.Radiothearphy protocol pre & post op?
My choice is radiation the morning before operation( experimental evidence in literature)
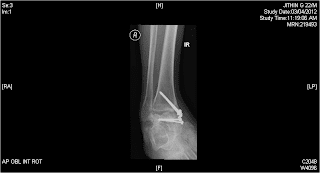
Below is a similar case I discussed before, So far I could trace only the preop and one post op at 3 months. will trace the entire series in a few days once I get back to get the whole story.
Dr. Mojieb's Comments are added below
1- Would pre operative aspiration add value too to ascertain the possibility if this being post sepsis or not
2- Any role for Posterior Approach ???
That might give u a better opportunity of visualizing & protecting the hip abductors.The only issue will be, where to osteotomize the ankylosed hip which I think u can do it a bit low , just above the lesser trochanter , this will help you retract the whole femur + abductors out of your way than ream away the acetabulum piece meal initially than as the landmark for the ant+ post columns become available u can place the Homan.
I like your idea about the neurovascular structure concern & the use if laser for bone cauterization
I personally have not used laser before but seems to be a great idea.
Please give your views and comments
54yr male diabetic presented with bilateral stiff hip since one yr,slowly progressive to total stiffness since last six months.
History of septicemia with multiorgan failure one n half yr ago,recovered well but unable to stand or sit due to bilateral stiff hip.
His question are as follows? My comments below are open to your valuable comments and views
1.Is THR only option?
With the sort of long standing Ankylosis the articular cartilage nutrition suffers and result in fibrous or bony ankyloisis. The question whether this was the result of septic arthritis or due to neuraxial injury could be partly answered by ESR, CRP and intraop frozen section. Being a diabetic an HBAIC is advised. IF proven to be infected could consider girdlestone with local antibiotic delivery could be a choice before THR. If not A THR with the largest possible head to avoid dislocation
2.What will be the status of Abductors after removing HO?
I would go dead lateral, split the TFL with anterior and posterior with bone slivers from the G. Troch. Do a neck ostetomy and remove the head, Ream or piece meal. After this the bone anterior and posterior can be removed slowly exposing the bone subperiosteally and reove all the impinging bone. You want to watch for N/V damage palpating vessels and preop MRI angio if needed to asses where the vessels are embedded if needed. The all important homan's retractor, electroquatery helps exposing the HO. The one similar case i did had a compartmental syndrome of thigh and femoral neurpraxia which recovered partially in 6 months. The contralateral hip was done 6 months later and laser was used toquarterise the bleeding bone to avoid compartmental syndrome. Those days we did not have any local thrombin delivery to stop bleeding if possible.
3.When should i do the second hip(gap between two THR)?
I would wait 3 to 6 months only for recovery
4.What are the chances of recurrence? In my only experience of a bilateral case the xrays below the hip failed with a psuedo tumor due to MOM articulation with an XL head.
5.Radiothearphy protocol pre & post op?
My choice is radiation the morning before operation( experimental evidence in literature)
Below is a similar case I discussed before, So far I could trace only the preop and one post op at 3 months. will trace the entire series in a few days once I get back to get the whole story.
Dr. Mojieb's Comments are added below
1- Would pre operative aspiration add value too to ascertain the possibility if this being post sepsis or not
2- Any role for Posterior Approach ???
That might give u a better opportunity of visualizing & protecting the hip abductors.The only issue will be, where to osteotomize the ankylosed hip which I think u can do it a bit low , just above the lesser trochanter , this will help you retract the whole femur + abductors out of your way than ream away the acetabulum piece meal initially than as the landmark for the ant+ post columns become available u can place the Homan.
I like your idea about the neurovascular structure concern & the use if laser for bone cauterization
I personally have not used laser before but seems to be a great idea.